
Ronald Shapiro, MD, Valarie Calander MD, Hair and Scalp Diseases Hodinskiy ,Mc Micheal Chapter 13: 176-195
SOCIAL IMPACT OF HAIR LOSS
Although, there are those who accept hair loss gracefully, for the many it is the causes of significant social and psychological stress. Concern over hair loss has been documented throughout history. Recently, a 5000-year old body from the Neolithic Age was found frozen outside of Austria. The frozen body had a neatly trimmed beard and closely cropped hair- so obviously the appearance of hair was important as far back as 5000 years ago. One of the oldest known medical texts is an ancient Egyptian papyrus scroll. Among its remedies is an ointment for restoring hair loss consisting of equal parts crocodile and hippopotamus fat. The ancient Greek physician Hippocrates interest in hair loss was stimulated by his own baldness- and indeed the name for the permanent fringe of hair that encircles the back and sides of the head has sometimes been referred to as the “Hippocratic Wreath”. We are all familiar with the story of Samson and Delilah, perhaps the most famous “hair equals virility” story of all time.1
In modern times over 50% of men and 25% of women will suffer from some degree of hair loss. 2,3,4 Over 2 Billion dollars a year are spent on various treatments for hair loss. No other facial feature will change ones appearance as much as hair loss.
Dermatologists and other physicians are often asked to evaluate patients for hair loss. Apart from establishing the etiology of hair loss, patients want to know how the hair can be restored. Hair transplantation has become a significant treatment tool in the armamentarium for hair loss. A survey by the International Society of Hair Restoration (ISHRS), estimated that over 80,000 hair transplant procedures are performed yearly in the United States alone. It is ranked as the second highest cosmetic procedures done on men.
In this chapter we review the advances that have occurred in hair restoration procedures as wells as examine procedures for areas not commonly thought of as being treatable such as eyebrows and eyelashes. We also look at various concerns that dermatologists and other physicians may have in deciding whether patients should be referred for possible hair replacement particularly as it relates to cicatricial and non cicatricial forms of alopecia. Additionally we review special considerations involved in treating Asian and African American patients.
HISTORY AND EVOLUTION OF HAIR TRANSPLANTATION
Historically, Male Pattern Baldness (MPB) is the most common indication for hair transplantation. It is caused by exposure of hair to the androgen Di-Hydro-Testosterone (DHT) which is a metabolite of testosterone created when testosterone reacts with the enzyme 5-alpha- reductase.5 When susceptible scalp hairs are exposed to DHT they become finer and shorter with each recurring growth cycle eventually leading to baldness. The severity of MPB varies dramatically and can be as mild as minor recession of the hairline or as severe as complete loss of the hair on the superior aspect of the scalp. Genetically determined differences in the sensitivity to DHT explain these variations between people. However even in the most severe case of MPB, hair loss does not occur in the horseshoe shaped ring of hair in the occipital and lateral fringe areas of the scalp because this hair is not sensitive to the effects of DHT.
The first description of hair transplantation was actually written by Dr Okuda in Japan in the 1930s. He used hair transplantation to treat burn victims during WWII. However records of his work were lost after the war. In 1950 Norman Orientreich MD rediscovered the process and successfully performed the first hair for transplant in the United States for patients with MPB. 6,7 He proved when “donor” hair from the permanent horseshoe shaped fringe area on the back and sides of the head was moved to the balding “recipient” area on the top of the scalp that it continued to grow and did not fall out. Donor hair from the fringe area remains insensitive to DHT and it this property of donor hair and not local properties in the recipient area that enables transplanted hair to grow. Orientreich called this property “donor dominance” and it is the property that makes hair transplantation possible.
It is important to point out that this fringe of donor hair is a finite and limited area that can only produce a finite and limited amount of donor hair. The concept of a limited donor supply is an important concept in hair transplantation as it places a limit on what we can accomplish.
Although Orientreich demonstrated that we could move hair and it would indeed grow, the original procedure often created an unnatural look and therefore had limited application. The desire to improve naturalness has led to many improvements in the technique, more natural results and a broader range of applications. The following is a brief over view of the evolution of the procedure.
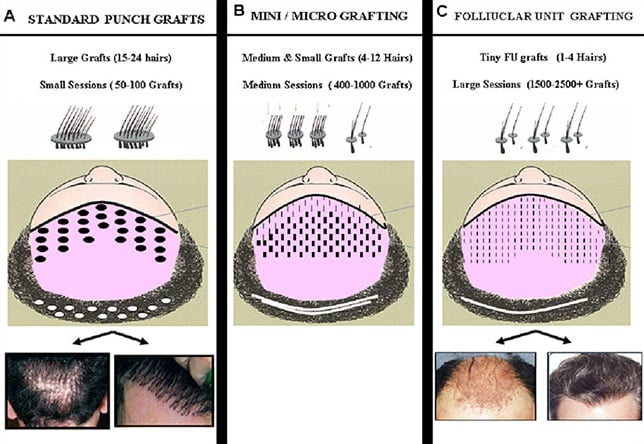
STANDARD PUNCH GRAFTING (Fig. 1A)
From 1950 to the early 1980s the only procedure available to the public was the technique made popular by Orientreich called Standard Punch Grafting.6 This procedure used large circular grafts (often called “plugs”) harvested by round punches. Each graft was about the size of a pencil eraser and contained as much as 20 to 30 hairs per graft. Only 50-100 of these grafts were used at a time and they were placed into round recipient sites also created by punches. There were intrinsic problems with this technique that led to unnatural results. First of all the large plugs had to be spaced rather far apart due to the constraints of blood supply and this led to the “dolls head” look commonly associated with transplants of the past.
The only way to at least partially resolve this dolls head appearance was to do multiple procedures in an attempt to fill in the gaps between the plugs. Many patients frustrated and disappointed with the initial results simply did not finish the process. Even if patients did finish the process other problems with naturalness occurred over time due to the inefficient use of the limited donor supply. To fill in the gaps, physicians were forced to use up the entire donor supply in a very small area. Very unnatural islands of grafted hair became noticeable over time as hair loss progressed and receded away from these heavily grafted areas.
To make matters worse there was now no donor hair left to fix the situation. It was during this time that physicians learned to appreciate and take into account the progressive nature of hair loss when planning hair transplantation in patients with MPB. Another problem with this technique was that it wreaked havoc with the donor area. The punches used to harvest these “plugs” from the donor area often left a scarred checkerboard pattern in the back of the head. The technique of Standard Punch Grafting is obsolete and no longer used. Unfortunately many patients with this old technique are still walking around and people mistakenly think that they represent hair transplants today.
COMBINATION MINI-MICRO GRAFTING (Fig. 1B)
The desire to improve naturalness led to the use of smaller grafts. By the late 80’s and early 90’s a technique called Mini-Micro grafting became the standard. Graft size had been reduced to 4-12 hairs per graft. Small slit incisions were now used for the recipient area instead of round punches. The decreased vascular trauma associated with these smaller slit incisions enabled a larger number of grafts to be placed closer together in a single session. Procedure size increased to an average of 400 to 800 grafts per session. Donor harvesting and graft preparation techniques improved also. Donor tissue was no longer harvested with individual round punches but rather from a single strip of donor tissue (a process called strip harvesting). The harvested strip was subsequently divided into individual grafts. This produced less scarring leaving behind a single linear scar rather than a checker board pattern. Strip harvesting also increased the total amount of hair that could be harvested from the donor area. Mini-Micro grafting was a vast improvement over Standard Punch grafting but the results were still not totally natural under all conditions and room for improvement still existed.
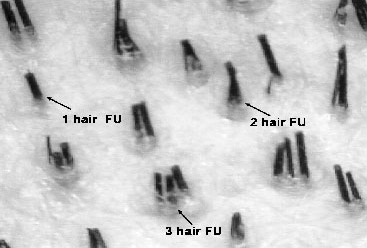
FOLLICUAR UNIT TRANSPLANTATION (Fig. 1C)
By the mid 90’s Follicular Unit Transplantation (FUT) became the state of the art procedure used in hair transplantation. This revolutionary advance occurred when physicians observed that hair grows and exits the scalp in tiny, naturally occurring groupings of 1-4 hairs called follicular units. (Fig. 2) With this observation physicians began using microscopic magnification to create grafts that keep these natural groupings intact.8, 9 These 1-4 hair grafts, called Follicular Unit (FU) grafts are so tiny they can be placed in micro-incision about the size of a needle. The reduction in graft and recipient site size allowed for larger numbers grafts to be placed closer together with less danger of vascular trauma. Procedures consisting exclusively of FU grafts could range from1500-2500 depending on the size of the area being treated. FU grafts can be placed at densities of about 20-30 grafts/cm which is significantly closer than with mini grafts. These tiny grafts replaced hair with the same size groupings found in nature. By placing large numbers of these grafts in patterns that mimic nature a totally natural and undetectable result could be now be produced.
As a side benefit , the degree of naturalness produced with FUT enabled physicians treat situations that could not be treated before and expanded the application and use of hair transplantation. FUT enabled more delicate work such as, eyebrows, eyelashes, beards, mustaches to be done. FU grafts have also been found to be successful in some cases of traumatic and disease induced scarring alopecias.
Most physicians now use exclusively FU grafts when performing hair transplantation procedures. However, for the sake of completeness, is should be mentioned that some physicians still use a combination of mini-grafts and FU grafts in selected situations. They feel that in selected situations, combining FU grafts with slightly larger mini-grafts can achieve better density; and can do so without noticeably sacrificing naturalness. This is an ongoing controversy in hair transplantation that has yet to be resolved.
SCALP REDUCTIONS, FLAPS, TISSUE EXPANDERS
Scalp reductions, flaps and tissue expanders are other tool that can be used to treat areas of alopecia on the scalp. These are much more aggressive procedures and have a greater degree of morbidity than hair transplantation. The results are often not natural. With the advent of follicular unit transplantation these procedures have fallen out of favor for purely cosmetic procedures as the results are not worth the morbidity. However they still have a place in the reconstruction and treatment of the more severe traumatic alopecia and should not be forgotten. The morbidity is warranted when severe traumatic alopecia’s (from burns, accidents, congenital abnormalities, etc) have created severe aesthetic deformities that limit social interaction and the quality of life. Often reductions or flaps are in combination with transplantation to create optimum results.For example a reduction may be used to excise the majority of the scarred area with transplantation being used to create a final natural look in the remaining exposed areas.
There are two flap procedures used purely for cosmetic purposes that deserve special mention.The first is a procedure used to treat the balding crown. It is called the Frechet Triple Flap and is performed by Dr Patrick Frechet in Paris France. It is a method of using a combination of serial scalp reductions in the crown followed by an elegant rotating flap procedure to cover a balding crown.[10]
The second procedure is the Female Hairline Advancement Flap made popular by Shelly Kabaker MD in San Francisco. It is a procedure where females with an unusually high hairline may have the hairline surgically pulled down rather than grafting a new hairline.11 In properly selected patients these two flap procedures are still useful. However over 90 percent of the procedure done today to treat alopecic scalps are done with follicular unit transplantation.
BASIC PRINCIPLES OF HAIR TRANSPLANTATION
Meeting a patients expectation of naturalness and density both now and in the future if hair loss progresses, are the two most important goals in hair transplantation. If we can achieve these goals the surgery will be considered successful. Achieving these goals takes both skill with the procedure but also requires setting proper expectations with patients. Understanding the following basic principles are helpful in understanding how to achieving these goals.
THE ISSUE OF NATURALNESS
Creating naturalness is in my opinion the most important goal in hair transplantation However, it important to note that simply using follicular unit grafts does not guarantee natural results. Knowledge of natural patterns and the ability be reproduce these patterns are also necessary. An analogy would be similar to using a small paint brush as a tool to paint delicate art. Having the small paint brush is not enough…one also needs to know how to paint.
THE ISSUE OF DENSITY
Meeting a patient’s expectation of density is the second most important goal in hair transplantation. By expectation of density we are referring to the area of baldness that can be covered and the degree of fullness that can be achieved in these areas. Meeting patients expectations of density can often be difficult for a number of the following reasons.
Poor Survival
FU grafts are very delicate and therefore susceptible to trauma and decreased survival. Cutting and placing large numbers of these very tiny grafts close together without trauma is technically difficult. There are many steps throughout the procedure (donor harvesting, graft preparation, recipient site creation and placing) where the grafts are vulnerableMany innovative techniques have been developed over the years to improve survival These will be discussed later when we go through the steps of the procedure. With the use of these innovations a skilled and experienced physician can minimize trauma and the survival rate can increase to be near 90-100%.
Limited Supply of Donor Hair
However, even with good survival there is another reason creating the “appearance” of fullness can be a challenge. This reason is that there is only a finite and limited amount of donor hair available to move from the donor area to the balding recipient area. The amount of donor hair available for transplantation can often be less than the amount of hair that originally existed in a balding area before hair loss started, especially in patients with extensive hair loss. Therefore, to some extent our hands our tied and in we simply cannot reproduce— at least hair for hair—the same mathematical density that existed before hair loss started. Consequently, a major goal in hair restoration surgery is to be able to create the “appearance” of fullness or the “illusion” of density at lower than normal ‘mathematical’ densities. Fortunately, this goal is achievable as explained below.
Creating the “Illusion” of Density
One explanation why we are able to achieve this goal is that a normal “illusion” of density or “appearance” of fullness can be maintained until we lose approximately 50% of our original hair. This long held and widely accepted dermatologic concept was verified in a study by Marritt who demonstrated that “parted” hair in a 1 cm area did not begin to appear “thin” or to “widen” until approximately 50% of the original hair was lost. This same principle applies in reverse when replacing hair. In other words we only need to replace hair to approximately 50% of its original volume to create an “appearance” of fullness.
Another principle that allows us to create the “illusion” or “appearance” of fullness at lower than normal mathematical densities is that the “appearance” (or “illusion”) of fullness is, not only determined by the quantity of hair in a given area, but also by the effectiveness of hair at creating this “illusion”. Stated another way, equivalent amounts of hair can appear thicker or thinner depending on how effective this hair is in creating the “illusion” of fullness. The following factors and characteristics have an influence on the hairs ability to create the “illusion” of fullness.
- Low Color Contrast Between the Scalp and Hair – When there is a low color contrast between the hair and scalp (such as with blond hair on light skin and black or brown hair on dark skin) the wavelength of light reflected from the scalp is similar to that of the hair shaft. This makes it more difficult to notice thinning and increases the illusion of density Products used to color the scalp exert their effect in the same manner.
- Hair Curl and Caliber – Curly hair and higher caliber hair is more effective at creating the appearance of fullness because these characteristics increase the amount of hair surface area, in a given volume of space, that is interposed between the scalp and eye.
- Angle of Hair Leaving the Scalp – The shingling effect that occurs when hair is placed at a more acute angle positions the hair in a manner such that more of the surface area of the hair lies between scalp and the eye. It also cause the hair to overlap creating a greater illusion of density.
- Orientation of Hair – It has been proposed that orientating grafts in what is called a “coronal” incision may create a greater illusion of density because this causes the hairs in the grafts to line up side by side instead of one on top of each other thereby creating more of a wall between the scalp and the eye.
An understanding of the above principles helps us deal with our patients in 2 very important ways. First it allows us to better predict and consequently educate patients about the degree of fullness they may achieve with a given amount of hair depending on differences in the curl, color, and caliber of the hair. It also gives us tools such as angling, shingling and different orientations that may help us to create a greater “appearance” of density with less hair.
Hair Loss Progression
One of the main difficulties facing physicians treating male and female pattern alopecia is that hair loss can progress at an unpredictable rate. Patients with mild hair loss today may have severe hair loss in the future. Physicians need to be careful to transplant hair in a pattern that will look natural not only today but also if the hair loss progresses and recedes away from the transplanted area. Areas of thinning that improved when transplanted hair was added to native hair may become thin again in the future as native hair is lost. Patients need to be educated about the possibility of needing more work in the event of progression. Physicians also have to leave enough donor hair has in reserve to treat any possible progression.
Adjunctive Medical Treatment
There are currently two FDA-approved medical treatments for hair loss, minoxidil (Rogaine®), and finasteride (Propecia®). In order to obtain maximum density now and in the future it is important use adjunctive medical therapy to preserve existing native hair. Medical therapy may bring back some lost native hair but just as important is slowing down or stopping future loss. The use of medical therapy can affect surgical planning in a number of ways. On occasion the response is so good that patients decide they don’t need surgery. On other occasions it improves the situation so a smaller less aggressive procedure is needed. Even if medical therapy is only minimally effective a small amount of regrowth can significantly improves the appearance of density in transplanted areas.
Minoxidil (Rogaine®) is a topical application approved for both men and women. It is available in two strengths which are 2% and 5%. It has been shown to either reduce hair loss or promote hair growth in about 80% of patients. Personal experience by me, and others, suggest that approximately 50% of men have their hair loss slowed, 35% continue to lose hair (i.e. no effect) and approximately 15% show some signs of regrowth. In men, 5% minoxidil has been shown to be more effective than 2%, demonstrating a dose-dependent response. 12, 13 It appears that minoxidil acts as a direct anagen-prolonging agent. A big problem with the use of minoxidil is compliance. The original product was oily and messy and the propylene glycol additive could cause irritation in patients. Recently a new 5% foam delivery system has been released without any propylene glycol. It is much easier to use and better accepted by patients.
Finasteride (Propecia) is a 1mg oral tablet taken daily that acts as a potent 5-reductase type-2 inhibitor. It blocks the conversion of testosterone to Di Hydro Testosterone and decreases levels of DHT by about 65 percent. It has shown impressive effects in both blocking further hair loss, as well as producing re-growth. The effects are greatest on the crown however it has some beneficial affect in the frontal area also. Five-year results showed that by hair-count, 65% of men stablalized or improved.14, 15 There is concern that the efficacy of Finasteride may wear off with time. However we have patients who have been on Finasteride for over 10 years with continued affects. We still don’t know what percentage of patients will continue to respond long term. Finasteride is not approved for use in women and a study by Merk on post menopausal women over the age of 50 did not show any benefit. There are a few small independent studies and anecdotal reports that suggest Finasteride may have some beneficial effects in younger women. However, the use of Finasteride is contraindicated in women of the child bearing potential because of possible birth abnormalities that could occur to the fetus of pregnant women taking Finasteride.
In men Finasteride has a very low side affect profile. The most common concerns are sexual side affects, gynecomastia and decreased sperm count. Even though the incidence of sexual side affects was low (1.8 percent with Finasteride compared to 1.6 percent in placebo) and reversible when stopped, it is still unsettling to a few men.
Dutesteride (Avodart®) is a new 5-reductase inhibitor that blocks both type 1 and 2 versions of the enzyme. It decreases levels of DHT greater than 90 percent and is felt to be more effective than Propecia. However it has a very long half life and the side effect profile is thought to be worse than that of Finasteride. It is not released for the treatment of male pattern baldness yet some hair transplant clinics use it off label on patients that are not responsive to Propecia with warning about the potential side effect.
Education to Set Expectations
Even if work is done perfectly a patient will not be happy if the results he receives are not what he expected. In order to insure expectations are realistic the following steps need to be taken:
- Evaluate available donor supply both in terms of total amount and the characteristics of the hair that may influence its effectiveness at creating the appearance of density (color, curl, caliber etc). Every patient is different with donor supply ranging from 4000 to 8000 follicular units.
- Evaluate size of the area of alopecia that needs to be treated.
- Predict, as best as possible, how much progression may occur in the future. Every patient is different based on their age, current severity of loss, family history, etc.
- Evaluate the patient’s expectations and desire for coverage.
Evaluate if the patients expectations of density and coverage are possible with the patients donor supply. - Educate the patient about what is realistically possible now and in the future based on the donor supply.
- If the patients expectations are not realistic or achievable ……then he or she should not have surgery at this time!
It is important for hair transplant surgeons to be familiar with and be able to identify patients with body dysmorphic disorder (BDD). BDD is recognized as a psychiatric condition where a patient obsesses on minor or imagined defects in their appearance. This obsession may markedly interfere with the patients’ ability to form personal relationships or hold a job. If the “defect” is corrected by esthetic surgery, another “defect” will quickly be discovered. It is not uncommon for cosmetic surgeons including hair restoration surgeons to be approached by patients with BDD and they must become good at identifying these patients as they are not good candidates for surgery.
THE PROCEDURE
Follicular Unit Transplantation can be divided into 4 major steps: donor harvesting, graft preparation, recipient site creation, and placing of grafts.
STEP 1- DONOR HARVESTING (Fig. 3A)
The goal of donor harvesting is to remove scalp tissue from the permanent donor area in a way that limits transaction or waste of the hair. In addition we want to leave as small a scar as possible in the donor area. It is important to remain within the permanent fringe area when removing the donor strip. If we stray outside this area the grafts prepared may be lost as time progresses. The length and width of the strip harvested is based on the number of grafts needed, and the donor density. It is important to measure the skin laxity of the donor area before taking out the donor strip. Some patients have very tight scalps and this limits the width that can be taken safely. Patients with poor donor density and tight scalps are in general poorer candidates for surgery. The donor is taken as a single strip using either single scalpel or a two bladed scalpel Great care is taken to angle the blades to be parallel with the hair shaft in order to prevent transaction and damage to the follicular unit A new technique has been developed to help minimize the scar associated in the donor area with this incision. This is called a “trichophytic closure”. With this closure one edge of the wound has the epithelium trimmed away exposing the tips of the hair shafts. It is hoped that after suturing these hair shafts will grow through and camouflage any scar. If multiple procedures are performed over time, an attempt is made to include the previous scar in each incision in order to create a single scar.
An alternative form of donor harvesting called follicular unit extraction (FUE) has been advocated by some physicians. This technique involves utilizing a 1mm punch to harvest one individual follicular unit at a time. The driving force for the creation of this technique is the avoidance of a linear scar , possibly allowing patients to cut their hair really short without any evidence of surgery. It has been promoted as the “scar less” surgery. However number of patients develop hypo pigmented dots at the site of punches and this advantage is lost as the number of punch sites increases. Other drawbacks include an increased risk of transection with each blind punch (especially in patients with curly hair) and a limit to the number of grafts that can be done in a single session. Also it is more time consuming and considerably more expensive than strip harvesting. Therefore it has found limited popularity. However in patients that only need a small amount of grafts or who are extremely worried about the donor scar it does have some use. The indications may expand as the technique is improved and made more efficient.
DONOR HARVEST & GRAFT PREPARATION
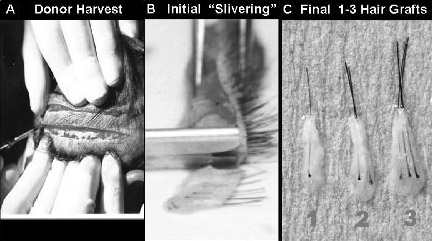
STEP 2-GRAFT PREPARATION (Fig. 3B ,C)
The harvested donor tissue is converted into grafts in two steps. The first and most critical step is called slivering during which the donor strip is cut into thin slices or “slivers” each about the width of one follicular unit. It can be visualized as similar to slicing a loaf of bread. It is important to use a dissecting microscope during this step to avoid transection. These slivers are then further dissected into individual 1-4 hair Follicular Unit grafts. The different size grafts are then separated and placed in different piles so they can be selectively distributed in the recipient area later. They are placed in a cooled saline until they are ready to be placed.
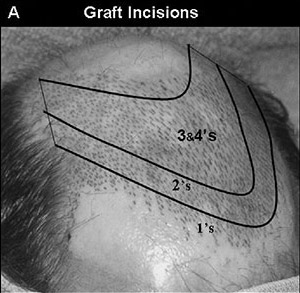
STEP 3-CREATING RECIPIENT SITES (Fig. 4A)
While the grafts are being cut, usually by highly trained assistants, the physician is making the recipient site incisions. Recipient site incisions vary in size from .7 – 1.2mm wide with the smaller incisions used for the 1-2 hair grafts and the larger incisions used for the larger 3-4 hair grafts or hair that is tightly curled. A number of different instruments can be used to make these incisions. The author used a specialized blade cutter that can be adjusted to create blades that vary in size. It is important for the physician to test the recipient sites to make sure the grafts fit properly and adjust the size of the blade if necessary. While making recipient site the physician needs to create a pattern that imitates nature. The incisions also have to enter the scalp at the same angle and direction as normal hair. They need to be made at the proper depth in order limit damage to deep vessels. If a patient is only thinning in an area and has pre-existing native hair, the physician needs to take care to avoid transecting these native hairs. Using true surgical loops for magnification aids in this.
RECIPIENT SITES AND PLACING
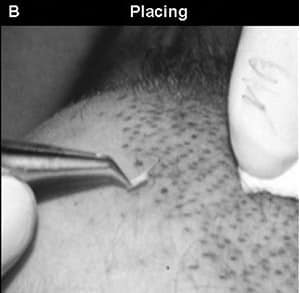
STEP 4–PLACING (Fig. 4B)
The ability to place grafts successfully is a critical step in the hair transplant procedure. The potential for graft trauma or dehydration occurring at this step is high. Placing a large number of tiny grafts into small incisions without trauma is technically difficult. The standard procedure is to use fine tipped micro-jewelers forceps to grab the graft at their base and then gently slide it into the incision. The use of surgical loops for magnification helps with this step. There is a tendency for grafts to get dehydrated if the process takes too long. Keeping grafts moist is critical as dehydration is probably one of the most common reasons for poor survival during placing.
POST- OP COURSE
Patients need to be educated about the post op course. In general there is very little immediate post op problems though a few patients may develop minor bleeding or infection in the donor area. There is some forehead swelling that occurs in about 20% of patients that usually lasts only 3 days. The transplanted hair usually sheds by about 2-3 weeks at which time the patient looks like he did before surgery. It begins to grow at about 3 months and between 3-6 months a significant change occurs and it is estimated that most patients have achieved about 60% of the affect by this time. Improvement continues for up to one year but by the end of a year usually what you see is what you get. Occasionally some patients may get a folliculitis around the 3 month mark when the hair starts to grow. This is easily treatable with topical compresses and if needed antibiotics.
In about 20% of patients a complication called “shock loss” or “telogen effluvium” occurs. This describes when a percentage of the native hair that was still present in the recipient area before surgery temporarily is traumatized, goes into a telogen effluvium. Usually this is temporary loss and the shocked hair will regrow. However, sometimes a percentage of the shocked hair will not regrow. There is more risk of this shock loss in patients that have only early thinning and a significant amount of pre-existing native hair. Shock loss is also more common in women. Patients with pre-existing hair need warned about this potential complication.
PRACTICAL APPLICATIONS OF HAIR TRANSPLANTATION
Male Pattern Baldness is the most common indications for hair transplantation. However with the advances made with follicular unit transplantation the indications have broadened. Women and ethnic groups such as individuals of African descent and Asians often seek out hair transplantation and have unique properties that need to be considered. Transplantation can now treat delicate areas of hair loss on the face such as eyebrows, eyelashes, beards and mustaches. Other indications now include scarring on the scalp from accidents, burns, and surgery. Although controversial transplantation can even be used to treat some forms of cicatricial and inflammatory alopecia’s. In this final section we will discuss both the common and less commonly thought of applications for hair transplantation.
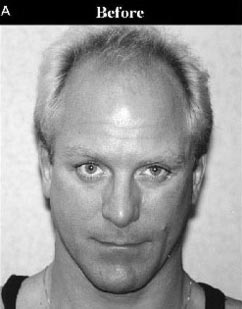
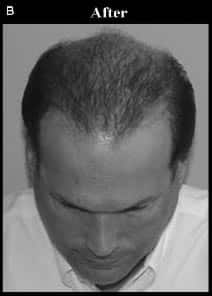
MALE PATTERN BALDNESS (Fig. 5)
Male pattern baldness (MPB) is the most common cause of hair loss in men and the common indication for hair transplantation. As stated earlier in order to have a successful hair transplant we need to meet the patient’s goals of both naturalness and density.
Creating naturalness is achieved by using 1-4 hair FU grafts to mimic patterns and distributions of hair found in nature. Creating a natural hairline is most important. A hairline should initially appear irregular, soft, and ill defined but gradually take on more definition and substance as it moves posteriorly. Creating too abrupt or straight of a hairline does not look natural and is a common mistake made by beginning transplant surgeons. To accomplish this goal only 1 hair FU’ grafts are in the anterior portion of the hairline with a shift towards 2 hair FU grafts as we move toward its posterior portion. Behind the hairline density is more important and a shift toward larger 3-4 hair FU grafts is made. This is called selective distribution of grafts and is an important technique used in hair transplantation. It is also important to make incisions at the angle and direction that follows the natural flow of hair.
The amount of density that we can ultimately create will depend on the severity of hair loss and the supply of donor hair. The severity of MPB varies dramatically and can be as mild as minor hairline recession of the hairline or as severe as complete loss of the hair on the superior aspect of the scalp.. Hair Loss is progressive at an unpredictable rate. It is very hard to predict how severe a pattern will develop in a patient when they are young. Family history helps a little but is not very reliable. Probably the best predictor is the age and severity at which hair loss begins. A patient that develops significant hair loss at a very early age will most likely end up with severe hair loss. while patient that only begins to recede in his 40’s or 50’s will most likely have less severe pattern.
Predicting and communicating the degree of density and the area of coverage that we can provide a patient is one of the most difficult skills to learn in hair transplantation. Since most patients have enough donor to cover the front half of their head we usually suggest that patients treat the front half first. When they are satisfied with the front we can move to the crown if there is donor left . The general dogma is to plan for worse case scenario and maximum hair loss. We can be more aggressive if a patient is older with minimal hair loss. . The most difficult patient to treat and the ones who need to be educated the most about realistic expectations are:
- Patients that want their hairline too low
- Patients that are just beginning to thin and don’t want to “see scalp”
- Patients with severe hairloss in both the front and crown who want full coverage everywhere
- Young patients with early hair loss in whom we cant be sure how severely they will progress
MALE PATTERN BALDNESS

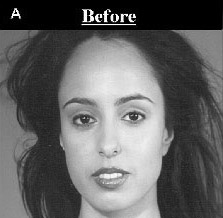
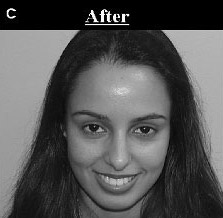
FEMALE PATTERN ALOPECIA (Fig. 6)
Hair transplantation has can be successful in for Female Pattern Alopecia and the number of females seeking hair restoration surgery is on the rise. In our society it is socially acceptable for a man to lose his hair. He may not like it, but at least male pattern hair loss is considered a variation of “normal”. After all, a majority of men have some degree of noticeable hair loss by the time they reach midlife. Hair loss in females is not as socially acceptable. With female pattern baldness, women feel “abnormal” and find themselves in a position that makes them extraordinarily uncomfortable.
The incidence of Female Pattern Alopecia (FPA) is greater than most people realize. Norwood recently reported that female pattern alopecia is as high as 30% in females over 30 years of age. Others have reported even higher incidences when females are carefully examined. 16, 17 One reason why this is not generally appreciated is that females are very good at hiding thinning with hairstyles, products and hair pieces.
The pattern of hair loss in FPA is different then MPA in that the hairline is usually not affected but there is diffuse thinning in the central scalp behind the hairline. Ludwig and Olsen described the pattern slightly differently. Ludwig described FPA as occurring in a caudal and centrifugal pattern in which hair in the hairline is maintained, though it may thin to varying degrees. Ludwig created a scale in which she divides FPA into Ludwig Type 1, Type 2 and Type 3 with severity getting progressively worse as we move from 1 to 3. Olsen described a “Christmas tree” pattern of loss which begins as a “widened part” but evolves into a zone of hair loss that is widest anteriorly at the hairline and gradually narrows, with ragged borders, more posteriorly.
Females have some special issues that need to be addressed before deciding if they are a good candidate for surgery. First of all, females are prone to other etiologies of hair loss. If there are any signs and/or symptoms suggestive of an endocrine, metabolic or dermatologic cause, they should be investigated and treated appropriately. It is also important to rule out temporary hair loss caused by severe emotional or physical stress leading to telogen effluvium. However the majority of females seeking transplantation for hair loss have no apparent cause other FPB.
Females are much more susceptible to the post operative complication of “shock loss” or “telogen effluvium” of existing native hair still present in the recipient area. Post operative shock loss occurs when pre-existing native hair is triggered to go into a telogen (resting) phase by the local stressors of surgery. In men this can occur from 10% to 20% of the time while in females it occurs more frequently, almost 30% to 50% of the time. In general this shock loss is temporary, occurring about 2-3 months after surgery and resolving in about 4-6 months. However in some situations it does not totally resolve leading to a less dense result. Women need to be warned about this before surgery.
As with MPB, females must have appropriate expectations and enough donor to meet those expectation to be considered a good candidate for surgery. Females who are Ludwig Type 3 with severe hair loss may not be good candidates because they often have significant thinning that extends over the entire scalp including the parietal and occipital donor areas. They simply don’t have enough donor hairs to perform a procedure. At the other extreme, females with very mild hair loss may also not be good candidates. Females with early thinning often want the full head of hair they had when younger and want to get to the point of “not seeing scalp”. They need to understand that this is clearly an unrealistic goal.
Transplantation in these situations may actually make matters worse as the surgery may cause the loss of more pre-existing hair in the recipient area than it adds. The best candidate is a female with moderate hair loss that is easily noticeable when she exposes the area. These females are usually very realistic about their goals. Obviously, all of them would like their hair to be as thick as possible but most are thin enough to appreciate a moderate degree of increased thickness in the affected area that allows for better styling.
In addition to FPB, other common indications for hair transplantation in females are; the lowering of abnormally high hairlines either from heredity or after a brow lift; the creation of, eyebrows and eyelashes, and for the treatment of scars secondary to trauma or cosmetic surgery. These are discussed in more detail later in this chapter.
The possibility of hair transplanting in females should not be overlooked As many females today can expect excellent results.
FEMALE PATTERN BALDNESS


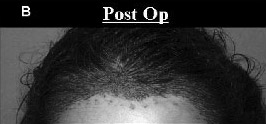
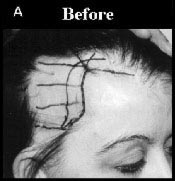
FEMALES WITH HIGH HAIRLINES (Fig. 7)
Another abnormality quite commonly found in females is genetically high hairlines that give the appearance of a large forehead. This may be the result of heredity or secondary to a brow lift. Women with this situation feel uncomfortable wearing their hair up or back and often wear bangs. Hair transplants are an excellent tool with which to lower the hairline. An alternative method of lowering the hairline is with the hairline advancement flap discussed earlier in this chapter.
HIGH FEMALE PATTERN HAIRLINES
EYEBROWS (Fig. 8)
Eyebrows play an essential role in facial aesthetics. Many women and some men seek help for thinning or absent eyebrows. With the refinement in follicular unit transplantation normal appearing eyebrows can often be restored.18 Loss of eyebrow hair may be due to trauma such as burns and avulsions; medical conditions such as hypothyroidism; or genetics. It may also be self inflicted due to long term eyebrow-plucking , or trichotillomania which is an obsessive-compulsive hair pulling disorder. Approximately one-third of patients attribute their thin eyebrows to inheritance and are born with them. It is important to treat and stabilize any underlying condition before transplantation. Enough time needs to pass after treatment to allow any potential re-growth of native hair to occur. Prior permanent make-up or tattooing is not a contraindication to eyebrow transplantation as the hairs will cover the tattoo. If the tattoo is to be removed it should be done so before transplantation. If the eyebrow tattoo was placed in an unaesthetic location, which extends outside the normal boundaries of the eyebrow, it can be surgically removed leaving a fine line that can then be easily concealed with the transplanted hair.
It is important understand the normal shape and patterns of eyebrows in order to recreate these shapes. The eyebrow can be divided into three parts; the medial portion is the head; the central portion is the body; and the lateral portion is the tail. An arch occurs along the eyebrow in women. The direction and density of hair is different in each of these parts. The hair is less dense and directed upward in the medial head. The hair is most dense and is directed more horizontally in the in the central body. However, in the body, the cephalic-most hairs tending to grow at a slightly caudal angle, while the caudal-most hairs tend to grow at a slightly cephalic angle, resulting in a cross-hatching affect and a greater illusion of density. In the tail hairs are less dense once again and directed horizontally. Only 1 and 2 hair grafts are used in the eyebrow with the 2 hair grafts designated for the thicker body of the eyebrow. Typically 200-250 grafts are transplanted into each eyebrow. These hairs are harvested from the occipital donor area as with any FUT procedure. The recipient incisions have to be angled very acutely to ensure the hairs lay flat against the skin and don’t stick out. Patients have to be told that the hair will grow long like normal scalp hair and that they will need to trim the hair to the desired length on a regular basis. If after surgery the shape of the eyebrow is not exactly what the patient wanted it can be sculpted afterward with electrolysis. Most patients get excellent results and are extremely grateful.
EYE BROWS


EYELASHES (Fig. 9)
Eyelashes have important an anatomical function of shielding the eye from injury-for example, from dust and grit. Eyelash transplants are usually reserved to treat functional total absence of the eyelash from disease or trauma. Eyelash loss can be due to a number of causes including:
- Facial injury and scarring from traumatic events or surgery
- Self inflicted due to eyelid tattoos, long-term use of false eyelashes, or trichotillomania;
- Medical disorders such as thyroid disease, lichen planus, and alopecia areata
The documented history of eyelash transplantation begins about 90 years ago with Dr. Franz Krusius, a German physician published his technique for reconstruction of lost eyelashes. In 1980, Emmanuel Marritt, MD, published his technique for transplantation of single donor hairs from the scalp into the eyelid for eyelash reconstruction. In the same year of 1980, Robert Flowers, MD, reported a “pluck and sew” technique of eyelash reconstruction. Marcelo Gandelman, MD has been demonstrating a modified version of this technique at hair transplantation workshops for the past 15 years.
The potential for serious complications exist when performing eyelash transplantation. These include lid infections, distortion of the lid, injury to the tarsal plate, and misdirected hair damaging the cornea.
Recently eyelash transplantation has been promoted for cosmetic enhancement of thinning eyelashes not due to trauma or disease. It needs to be said that there is controversy over the appropriateness of doing this do to the potential complications. Many recognized authorities in eyelash transplantation believe it should continue to be reserved for medically necessary eyelash replacement. However very delicate innovations have been made in the technique that allow better control of hair direction as well as more gentle insertion into the lid margins. The particulars of the technique are as follows. A small amount of scalp tissue is removed from the back of the head and used as a donor source for the eyelashes. About 30 hairs will be used for each eyelid. Only very fine single hair grafts are used. In contrast to other hair transplant procedures the hair shaft is left long like a piece of thread. This hair shaft is threaded through an opening at the back end of a very fine specialized curved surgical needle. The needle is then threaded through the top of the eyelid exiting through the tarsal plate at the point were normal eyelashes emerges. An attempt is made to follow the natural upward curve of the eyelash. As physician gain more experience with this technique it may become more acceptable to be used for cosmetic indications alone. 19
A class of drugs known as prostaglandin analogues have engaged interest for their potential use a medical approach to eyelash enhancement. The best known of these drugs is latanoprost, currently administered in eye drops to treat glaucoma. Ophthalmologists noted that latanoprost stimulated growth of existing eyelashes and darkened the eyelashes of treated patients. The effect has been studied as a possible medical approach to increasing the appearance of greater eyelash density. Side effects include blurred vision, eyelid inflammation, and a temporary burning sensation. The use of prostaglandin analogues for reasons other than glaucoma treatment has not been thoroughly investigated. Their use for eyelash enhancement should be approached with great caution.
EYELASHES



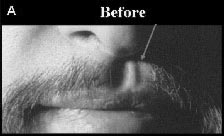
BEARDS AND MUSTACHES (Fig. 10)
Many men have bald spots or weak patches of hair in their beard or mustache. Follicular unit transplantation is ideal for filling in these areas. Normal facial hair usually consist of very thick and coarse 1 hair units. It is hard to find this degree of coarseness in the occipital donor area . Therefore 2 hair graft are usually used instead of 1 hair grafts in an attempt to match the thinness of the coarse beard hair. A common use for this procedure is to cover the defect resulting on the lip from a cleft palate repair.
MUSTACHE

TRANSPLANTING INTO SCAR TISSUE CAUSED BY PHYSICAL TRAUMA (Fig. 11,12,13)
Hair Transplantation can be used to treat areas of scarring on the scalp caused by different types of physical trauma. These could include scars caused by burns, explosions, accidents. Sometimes the scarring is iatrogenic and produced by surgical procedures such as face lifts, brow lifts, radiation treatment; or removal of a scalp tumor such as a hemangioma) Special considerations are needed when transplanting into areas of scarring. 20
The issue of adequacy of the blood supply to the scar tissue often arises. In addition to leading to poor graft survival, this limited blood supply can potentially leave the recipient area more vulnerable to infection, further ischemia and necrosis. Although these are legitimate concerns, experience has shown that the blood supply in scar tissue is often sufficient to accommodate the appropriate placement of FU grafts. However, certain precautions and modifications should be taken. Some physicians have recommended assessing the blood supply by sticking the tissue with an 18-gauge needle and waiting for the appearance of blood. If none appears after a few minutes, one should be extremely cautious and consider test grafts in the area before committing to a larger procedure. Smaller grafts and in particular FU grafts should be used when transplanting into scar tissue. FU grafts, with their associated small recipient sites, have the greatest chance of survival and the least chance of causing ischemic injury in scar tissue. In general, one should always perform the first transplant with a smaller number of grafts placed further apart so as not to stress the blood supply. It is also prudent to wait longer in between sessions. With scar tissue it is better to plan on doing multiple, smaller sessions that succeed rather than one large session that fails. Although not proven, some physicians suggest that the use of a 2% to 5% solution of Rogaine for one week pre-operatively and five weeks postoperatively may improve the blood supply, and the odds of a successful transplant. Theoretically, the use of pentoxyphylline (Trental®) 400 mg, three times daily with meals, for at least two weeks prior to surgery, may also provide greater oxygenation to the tissue.
BROW LIFT SCAR

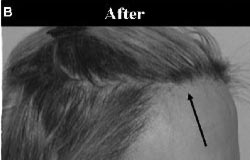
Not all scars are the same and scar thickness can have an affect on transplantation. Some scar tissue is thick and tough, while other scar tissue is thin and friable. With thick hypertrophic scars, there is concern that the incisions will not gain access to the blood supply. In these situations one should err on the side of making the incisions slightly deeper. Transplanting into thin atrophic scar tissue, such as that created by post-radiation injury, creates a different, and in our opinion, a more difficult problem. The recipient area in this thin, poorly vascularized tissue is more prone to ischemia. In addition, the shallow skin makes it difficult to create incisions deep enough to house even tiny FU grafts. Making the incisions at a more acute angle can increase the length of the incisions, and create a posterior “pocket” to house the graft. Carefully using a small amount of tumescent solution (without epinephrine) can temporarily distend the skin, making it easier to create these more acutely angled incisions.
On several occasions, we have noticed that after the first conservative transplant into an area of atrophic scarring, the tissue characteristics improve and become more favorable for a second transplant procedure. The tissue becomes thicker and suppler. It may be that the FU grafts act like multiple tiny skin grafts, and also may stimulate angiogenesis.
One should always consider surgical excision as an alternative or adjunct to transplantation for areas of alopecia in the scalp. If the area of scarring is relatively small, and the surgeon is confident that the scar can be removed by an excision alone than this should be considered. If an area of scarring is very large sometimes it is better to first excise a portion of the scarred area, leaving a smaller area to be transplant.
3RD DEGREE BURN


RADIATION SCARRING FOR CANCER THERAPY



TRANSPLANTING INTO CICATRICIAL ALOPEICIA (Fig. 14)
The term “cicatricial” contains the Latin root “cicatrix,” which means “scar resulting from the formation and contraction of fibrous tissue.” Historically, dermatologists have used the term cicatricial alopecia to refer to scarring alopecia caused by inflammatory disease processes such as, central centrifugal cictricial alopecia (CCCA) , pseudopalade, lichen planopilaris, frontal fibrosing alopecia, discoid lupus erythematosus, etc. Transplanting into inflammatory cicitricial alopecia is controversial. 20
The current philosophy amongst hair transplant physicians when transplanting patients whose scarring is the result of inflammatory disease processes is to be certain that the disease process has “burned out” before undertaking the procedure. A general rule of thumb has been to wait until there are no signs of active disease for approximately one to two years. It may be appropriate to consult with a dermatologist and/or obtain a biopsy from the area to be transplanted to ascertain if the inflammatory or infectious process has subsided.
Obviously the concern amongst transplant physicians is three fold; that the disease process will reactivate and destroy the newly transplanted hair; that the transplant procedure may possibly reactivate the disease process and; that the survival rate may be somewhat decreased compared to grafts placed in normal tissue. There are no scientific studies that address these issues. There is however a large body of empirical evidence in the transplant community demonstrating that grafts will grow successfully in burned out areas of cicitricial alopecia.. Patients are grateful for the cosmetic improvement. They often accept the risk that the growth may be poor or that they may lose grafts if the disease process reactivates. It may be that these patients sometimes accept these risks because we are improving on an unnatural deformity, rather than trying to reverse the natural balding process. However, it is important to educate these patients before the procedure and warn them about the possibility of disease recurrence and a decreased hair survival rate.
In examining the patient, it is also important to be certain that the apparent scar is indeed a scar. For example, in rare instances, a basal cell carcinoma of the sclerosing type can mimic a scar. If there is any question about the diagnosis, the area should be biopsied.
LICHEN PLANOPILARIS

PATIENTS OF AFRICAN DESCENT
Patients of African descent often request hair transplantation to treat areas of alopecia. Hair characteristics of patients of African descent present a both advantages and disadvantages for the hair restoration surgeon. 21,22, 23 If the surgeon understands these characteristics and works skillfully with them then excellent results can be produced.
A major challenge in patients of African decent is that they have an unparalleled degree of curl to their hair (Figure 16). A significant disadvantage of this curl is that it is much more difficult to harvest donor tissue and prepare grafts without transecting and damaging the follicles. This can lead to waste of the limited donor supply. The counter balancing advantage of such an acute curl is that, compared to straight hair, each hair covers a greater amount of surface area in a given volume of space. This curve combined with another favorable hair characteristic (low contrast between dark hair and dark skin) make the hairs of patients of African decent much more effective at creating the illusion of density as compared with other races.
Modifications in strip harvesting have been developed in an attempt to minimize the problem of transection. One modification is infiltrating the donor area with a large amount of saline tumescence. The pronounced turgor that is created in the tissue may help straighten these follicles, as well as increase the distance between them, thereby decreasing the probability of transection. Another modification is to bend the surgical blade used for harvesting in order for it to better follow the curve of the hair below the skin. A final and more recent advancement is to harvest donor by using a scoring technique followed by blunt dissection. With this technique the skin is first scored with a scalpel to only a few millimeters below the surface. Then a spreading device is inserted and the two edges are spread apart.
LICHEN PLANOPILARIS

Another challenge in patients of African descent is that the density of hair in the donor area is significantly less than in Caucasians (60 Fu/Cm vs 100 FU/Cm) (24,25). If one were to only take into consideration the number of hairs/cm2, virtually all patients of African decent would be considered poor candidates for hair restoration surgery. However the density in the recipient area recipient area is also naturally lower, therefore, when restoring an alopecic area in a patient of African descent, one does not have to achieve as high a mathematical density as in Caucasians in order to have a successful result.
Post-traumatic keloid formation is more common in individuals of African descent than in Caucasians. A high index of suspicion is therefore necessary when transplanting these individuals. One should check for the presence of keloids in areas of high flexibility (elbow, wrist, shoulder, knee, etc.) as well as on the scapula area and the sternum.
Performance of a “keloid test procedure” should consider in patients who you suspect may form keloids. This is done by transplanting a single 2 mm round graft to an area at the border of the recipient area in hair bearing skin. A period of three months should then pass after which observation of the healing is made. If no keloid is seen, you can cautiously proceed with the surgery. Although keloids can occur and are a concern in practicality they are very rarely reported (26). Other postoperative concerns that can occur more frequently in these patients are cobblestoning, hypopigmentation and hyperpigmentation.
Making the incisions and placing the grafts is also slightly more difficult in these patients for the following technical reasons; the grafts have to be kept slightly larger due to the curl; the skin is tougher leading to more difficulty in placing; the incisions are harder to visualize due to the dark skin; and there tends to be more bleeding making it difficult to see. Therefore, the surgical instrumentation used in recipient site creation should be customized to accommodate the extent of the hair curl. Typically, the selected instrument should produce incision sites greater than 1.2- 1.5 mm in size. All of these challenges can be overcome with skill and experience.
In addition to typical MPB and FPB there are a few other causes of hair loss that are more common to this group. Traction alopecia is a common form of hair loss in black women and develops from the chronic use of specific hairstyles, such as tight braiding, pony tails and hair extensions. This form of alopecia is also common in Muslim Seiks who pull their hair back to fit in tight turbans. When this is done over a long period of time the hair loss can become permanent. It is amenable to hair transplantation as long as the underlying traumatic hair style and traction can be removed (Figure 17). Chronic chemical injury due to straightening products is another cause of alopecia that may become permanent over a long period of time. This is amenable to hair transplantation as long as the inciting cause is removed. Central centrifugal cicatricial alopecia is a type of scarring alopecia seen in all races and either gender, but is seen mostly in black women. Although controversial, the current feeling amongst hair restoration surgeons is that once this disease is no longer active it may be amenable to hair transplantation. This was discussed earlier in the chapter.


ASIANS
Hair transplantation in the Asian population is increasing in demand. A recent study by Pathomvanich found that the incidence of MPB in Asians is similar to that of Caucasians. This differs from previous studies that estimated estimated the incidence of MPB to be approximately one quarter that of Caucasians. The Asian patient has unique characteristics and demands that need to be considered when planning a hair transplant. 26
The forehead of Asians’ tends to have less of a frontal projection than and therefore appears wider and rounder than the forehead of Caucasians. Asians prefer a rounder hairline than Caucasians and this has to be taken into considerations during the consult when evaluating the realistic expectation of the patient.
Donor density in Asians is usually lower than that of Caucasians with a higher percentage of smaller 1-2 hair follicular units as apposed to 3-4 hair follicular units. . In addition there is typically a high color contrast between black hair and light skin in Asians. Both these factors of make it more difficult to create an illusion of density in Asians. On the other hand, the hair shaft diameter in Asians men is usually significantly greater than in Caucasians helping create a greater illusion of density with each hair. This counter-balances the problem of low donor density and high color contrast in Asians to some extent but not to the same degree that the extreme curl and minimal color contrast counter balances low density in patients of African decent.
The combination of thick, coarse black, hair on the white skin found in Asians makes the creation of naturalness more difficult in Asians. It was particularly difficult in the past when larger minigrafts were used. However with the exclusive use of FU grafts in these patients naturalness can be created. Meticulous placement of only single-hair FU grafts at the hairline is particularly important in Asians as their hair is less forgiving with respect to naturalness than finer, lighter curlier hair. With Asians patients it is often necessary to go an extra step and search for and select out a special population of the finest single hair grafts for use at the hairline.
Another area of concern with Asians is that any scarring that occurs in the donor area will be more visible than scars in Caucasians due to the high contrast between black hair and white skin. In addition Asians are more susceptible to keloid formation and hyper pigmentation than Caucasians but to a lesser but to a lesser degree than patients of African decent.
In spite of all these issues hair transplantation can produce good results in properly selected Asian patients. Low density and high color contrast is compensated for by the larger caliber follicles and the use of single unit grafts at the hairline.
REFERENCES
- Rassman W. A Brief History of Hair. A Comprehensive Guide to Hair Restoration. New Hair Institute.,1997 : 11-13
- Norwood, O.T. Male pattern baldness: Classification and incidence. South Med. J. 68:1359-1365, 1975.
- Hamilton, JB. Patterned loss of hair in man: types and incidence. Ann NY Acad Sci, 53:708-28, 1951.
- Venning, VA., Dawber, RPR. Patterned androgenetic alopecia in women. J Am Acad Dermatol, 18:1-73-7, 1988.
- Sawaya M, Price VH. Different levels of 5α-reductase Types 1 and 2, aromatase and androgen receptor in hair follicles in women and men with androgenetic alopecia. J. Invest Dermatol 1997; 109: 269-300.
- Orentreich, N. Autografts in alopecias and other selected dermatological conditions. Ann. N.Y. Acad. Sci. 83:463-479, 1959.
- Orentreich, N. Pathogenesis of alopecia. J. Soc. Cosmet. Chem. 11:479-499, 1960
- Bernstein RM, Rassman WR, Szaniawski W, Halperin A: Follicular Transplantation. International Journal of Aesthetic and Restorative Surgery 3:119-132, 1995
- Limmer BL: Elliptical donor stereoscopically assisted micrografting as an approach to further refinement in hair transplantation. Dermatologic Surgery 20:789-793, 1994.
- Frechet, Patrick. Scalp Extension. In: Unger W, Shapiro, R(eds) Hair Transplantation. 4th Edition. Marcel Decker, New York 2004:765-785
- Kabaker Shelly. Female Hairline Advancement Flap . International Society of Hair Restoration Surgery Annual Meeting Sept 2006 San Diego
- Whiting, D.A., and Jacobson, C. Treatment of female androgenetic alopecia with monoxide 2%. Int. J. Dermatol. 31 :800-804, 1992.
- Olsen E et al, A Randomized Clinical Trial of 5% Topical Minoxidil vs. 2% Topical Minoxidil and Placebo in the Treatment of Androgenetic Alopecia in Men, l Am Acad Dermatol, Sept
- Whiting DA. Advances in the treatment of male androgenetic alopecia. A brief review of finasteride studies. Eur J Dermatol 2001; 11:332-334.
- Whiting DA, Waldstreicher J, Sanchez M, Kaufman KD, Measuring reversal of hair miniaturization in androgenetic alopecia by follicular counts in horizontal sections of serial scalp biopsies: Results of finasteride 1 mg treatment of men and post menopausal women. J. Invest Dermatol. Symposium Proceedings 1999; 4: 282-3
- Ludwig, E. Classification of the types of androgenetic alopecia (common baldness) occurring in the female sex. Br J Dermatol, 97:247-54, 1977.
- Unger Robin Transplanting in Women: Unger W, Shapiro,R(eds) Hair Transplantation. 4th Edition. Marcel Decker, New York 2004:516-524
- Jeffrey Epstein, MD, FAC Eyebrow Transplantation Hair Transplant Forum 2006; Volume 16, Number 4 :121-123
- ISHRS Website reference for eyelash at ISHRS.ORG
- Shapiro R, Rose P, Transplanting into Scar Tissue and Other Areas of Cictircial Alopecia UngerW, Shapiro R (Ed) Hair Transplantation 4th edition Marcel Decker, NY NY 2004:606-609
- Meyer M Hair Restoration in Patients of African Descent UngerW, Shapiro R (Ed) Hair Transplantation 4th edition Marcel Decker, NY NY 2004:595-602
- Jerry Cooley, Hair Transplantation in Blacks, Haber B, Stough D,(Ed), Priocedures in Cosmetic Surgery Series, Hair Transplantation, Elsevier Saunders, 143-147
- Callender VD. Hair transplantation for pigmented skins. In: Halder RM. Dermatology and Dermatological Therapy of Pigmented Skins. Boca Raton, FL: Taylor & Francis 2006: 245-257.
- Bernstein RM, Rassman WR. The aesthetics of follicular transplantation. Dermatol Surg 1997;23(9):785-799.
- Sperling LC. Hair density in African-Americans. Arch Dermatol 1999;135:656-658.
- Brown MD, Johnson T, Swanson NA. Extensive keloids following hair transplantation. J Dermatol Surg Oncol 1990;16:867-869.
- Demkerng Pathomavanich, Hair Transplantation in Asians, Haber B, Stough D,(Ed), Priocedures in Cosmetic Surgery Series, Hair Transplantation, Elsevier Saunders, 149-152

