How Many Hair Transplant Graft Do You Need?
One of the most common questions a patient asks is “How many grafts do I need?”. The answer to this question will be different in each patient. In order to answer this, a patient needs a full consultation & evaluations where his/her goals are assessed and both their donor & recipient areas are evaluated. With this information, we can evaluate first, “What can be done” & second, “How many grafts will you need?”
What Can Be Done in the "Average" Patient for Hair Transplant
- The average patient has ~ 6000 grafts available in his/her donor area for transplantation.
- The average size of the balding area in a Type 5 patient is ~ 200 cm2. This can be divided into two equal parts:
- The hairline and front half which is ~ 100 cm2
- The back half and crown which is ~ 100 cm2
- The math dictates what you can do:
- Option 1: You can distribute the grafts evenly throughout the bald spots, which would create a uniform density of about~ 30 FU/cm2 (6000/200 =30). This is not recommended. It would create a diffuse thinning look that most patients are not content with. Most patients would like a higher density in the front half closer to 40 FU/cm2
- Option 2: You can put ~ 4000 grafts in the front half and 2000 grafts in the back half. This will create a density of 40 FU/cm2 in the front half and a density of 20 FU/cm2 in the back half and crown. In most cases, this will create the appearance of fullness in the front half and hairline. And a slightly thinning look in the back half and crown.
What this means is that the average patient usually has enough hair to create the appearance of fullness in the front and coverage but a thinning look in the crown. Usually it takes 2-3 hair transplant sessions to move 6000 grafts.
However, all patients are different. Depending on a number of variables, some patients can get more coverage while others have to accept less. There are patients who do not have enough donor hair to do their crown at all. In some cases, a patient is not a good candidate for surgery at all.
Variables That Determine "What Can Be Done?"
Donor density:
The more donor hair available, the greater area of baldness that can be covered. Conversely the less donor hair available, the less area that can be covered. Most patients can get at least 6000 grafts but there are those that only have 4000 and those that have as much as 8000. Sometimes it is hard to predict the exact amount a person will be able to get.
Scalp elasticity:
This only applies to Strip procedures and not FUE procedures. The more lax the scalp the easier it is to get a larger number of grafts and cover more area. The tighter the scalp the less grafts that can be obtained and the less area that can be covered. There are scalp exercises and a new medication called Vitrase that can help increase the laxity of the donor area.
Hair characteristics:
Patients with good hair characteristics (thick, wavy, light colored hair) can always do more than patients with poor hair characteristics (fine, straight, black hair on white skin).
Severity of balding pattern:
The more severe the balding pattern the larger the recipient area is and the more hair grafting will be needed. The less severe the balding pattern, the smaller the number of grafts needed.
Head size:
Some patients have extremely large heads while others have smaller heads. The former typically require more grafts.
Age and potential to lose hair:
The younger the patient, the more risk they are for having future hair loss and needing more grafts in the future. The older the patient the less risk of this. This is unfortunately unpredictable. Family history and exams can help but is not a definite conclusion because while it is usually predictable who will lose more hair, it is impossible to predict who will NOT progress or the rate and speed of progression. This means that when evaluating younger people with existing concerns of any type of hair loss, they always have to be prepared to do more work if they progress.
Willingness to take medications like Propecia:
Propecia is a prescription medicine to treat male pattern baldness by promoting hair growth. It is also effective at preventing progression of hair loss and limiting size of the recipient area. It does not work in every one but it works in most patients. A patient that takes Propecia will usually be able to obtain more coverage and a fuller look.
Pre-existing hair & early thinning:
Patients who have only mild thinning & pre-existing hair, whether young or older, are more difficult to do for a few reasons.
- First, the more pre-existing hair they have, the more difficult it is to make an incision in between this hair without directly damaging or transecting it. The good news is that skilled physicians using high magnification loops can usually get in between pre-existing hair without damaging it when it has thinned to about ¼ of normal density or about 25 FU/cm2.
- Second, even if not directly traumatizing the hair, indirectly the surrounding trauma and inflammation can cause a temporary “shock loss” or telogen effluvium of the pre-existing hair.
What is “shock loss”? All the hair on our head goes through a repeating growth cycle where hair grows for 2-4 years; then goes to sleep and sheds; before growing back in a few months to repeat the cycle. This shedding phase is called “telogen effluvium”. Luckily, only 10 % of our hair does this at one time. If all our hair was synchronized to go through this growth cycle and effluvium at the same time, we would be totally bald during this shedding phase. This is what happens when a bird’s molt regrows about 3 months later. “Shock loss” is when the indirect trauma from surgery “triggers the pre-existing hair to enter this shedding or “telogen” phase and fall out. This shock loss can occur in about 20% of patients no matter how skilled the surgeon or how gently the surgery is done. Typically, it all grows back in about 3-4 months as the shredded scalp hairs re-enter the growth phase of hair. However, a percentage may not grow back. The hair that does not grow back is felt to be weaker hair that was destined to be lost over the next few years due to natural progression of the patient’s balding process. The surgery just sped up the process in these hairs. - Third, even if no direct transection or indirect shock occurs over the 12 to 14 months it takes for the newly transplanted hair to come in, there can be simple, natural progression and loss of the pre-existing hair due to the patient’s underlying balding process. This occurs more often in patients that come in with a history of suggesting they were actively losing hair before surgery.
Understanding Pre-Existing Hair Loss
The net effect is that if a patient has early thinning and pre-existing hair, they can lose some of this hair and this will blunt the beneficial effect of the newly transplanted hair. For example, if a patient has a pre-operative density of 25 FU/cm2 (which typically looks thin) and does a transplant that adds about 25 FU/cm2, the final density is about 50 FU/cm2 (which typically looks pretty full). BUT THIS IS ONLY TRUE IF THE PATIENT DOES LOSE ANY OF THEIR PRE-EXISTING HAIR. If they lose some of their pre-existing hair, they may not get the degree of change they were hoping for. Any patient who does surgery with a significant amount of pre-existing hair has to be aware of this and know they may need more work in the future.
Pre-existing hair and degree of change: Another problem with transplanting into areas of pre-existing hair has nothing to do with losing this hair but rather the ability to notice the degree of change. When patients have very thin hair or are bald, it is very obvious to everyone in all situations that a change has occurred. On the other hand, with early thinning a patient may appear fairly full under many situations, and only on critical observation when they part the hair or look very close in a mirror can they notice the thinning. Therefore, after the procedure the change is much less dramatic and they can often mistake this for poor growth. Patients have to be educated and made aware about this circumstance.
How Many Grafts Per Procedure for Specific Areas of Hair Loss
Below are the ranges of grafts numbers typically recommended per procedure for specific areas of hair loss. This number assumes the patient will let us shave the area. If a patient has pre-existing hair in these areas but will not let us shave, we usually have to do about 500 less grafts. Most of these numbers will add ~ 30-35 FU/cm2 in the area transplanted, which is the density shown by most studies that has the most consistent survival. Some patients who started out with no hair in these areas will be content with this density; many will want a second session in these areas to increase the density closer to 40-45 FU/cm2. Patients with pre-existing hair will also need a second session if and when they lose this pre-existing hair.
Hairline
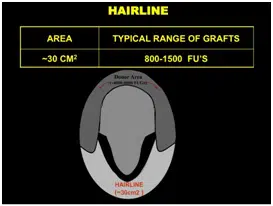
Hairline Patients often come in early when they are just early receding hairline. The area of the hairline can range from 10 cm2 to 30 cm2 if there is only a little temporal recession or if the weakness extends along the hairline. It will also change if we are bringing the hairline down and doing temporal points.
Typically, we recommend between 800 to 1500 grafts for a hairline. If we are doing Temporal points, it may add another 150 grafts per side.
Front Third
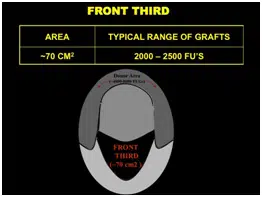
The Front third includes the hairline and the central core. It is approximately 70 cm2. It contains the frontal tuft, which is a very important area for creating the illusion of density.
Typically, we recommend between 2000-2500 grafts for the front third.
Front Half
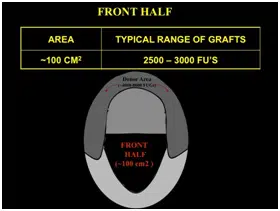
The Front Half is approximately 100 cm in size.
Typically, we recommend between 2500 to 3000 grafts when doing the front half.
Front Two Thirds
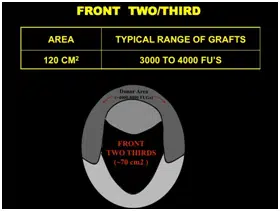
The Front Two Thirds is approximately 120 cm2 in size.
Typically, we recommend between 3000 to 4000 grafts when doing the front two thirds.
Crown
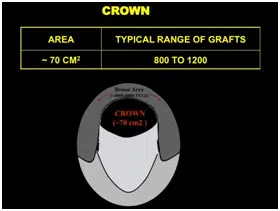
The Crown can range from 60 to 100 cm2. We typically do not want to place too many grafts in the crown until we are certain a patient has enough grafts to make sure his front two thirds will reach his expectation. However, in the average patient, it is usually safe to do at least 800-1200 grafts in the crown with the goal of turning a shiny bald spot into an area that just looks like it is thinning. But more than this number should not be done until we are sure a patient has enough grafts for the front.
We usually recommend between 800 -1500 grafts for the crown.



